Endometrial thickness is an important factor in implantation and pregnancy. In several studies, the minimum endometrial thickness for embryo transfer has been reported to be 7 mm. Several approaches have been tried to increase endometrial thickness for frozen-thawed embryo transfer (FET) cyclesbut as yet there is no consensus on the most effective method. Some FET cycles are cancelled due to thin endometrium despite routine treatment, and there is no recognized protocol for increasing the thin endometrium.
Chang et.al. 2015 has proposed a new approach for the treatment of thin endometrium, by infusion of Platelet Rich Plasma (PRP).
Growth Factors
Fresh PRP prepared from whole blood, collected from peripheral veins contains several growth factors such as
PRP has been used in several other medical conditions in e.g. sports injuries, diabetic foot healing, orthopedics, surgery and wound healing but its efficacy in endometrial growth has not been fully elucidated.
Treatment for Thin Endometrium
Hysteroscopic examination is performed before the cycle if it had not been done previously. Hormone replacement therapy (HRT) is started on the day of the cycle for endometrial preparation for IVF cycle Transvaginal ultrasound is performed by an expert gynecologist by one machine. Endometrial thickness is measured at the thickest part in the longitudinal axis of the uterus.
How is PRP Prepared?
PRP is prepared from patients own blood using a two-step centrifuge process.
Procedure for PRP Preparation:
On the 9th or 10th day of the menstrual cycle, the blood is processed as follows:
This procedure results in endometrial thickening, improved implantation rates and clinical pregnancies.
Who can Benefit from PRP Therapy for Thin Endometrium in Delhi?
Patients suffering from chronic thin endometrium can benefit from PRP therapy. The successful implantation depends upon the thickness and close dialog between the blastocyst and the endometrium.
Thin Endometrium may be Because of:
Persistent thin Endometrium should always be evaluated for;
“Several methods are performed for endometrial preparation in frozen-thawed embryo transfer (FET) cycles, and there is little consensus on the most effective route.
“On the 9th or 10th day of the mensural cycle, 17.5 ml of peripheral venous blood is drawn in the syringe that containing 2.5 ml of Acid Citrate A Anticoagulant solution (ACD-A) and centrifuged immediately at 1200 rpm for 12 min to separate the red blood cells.”
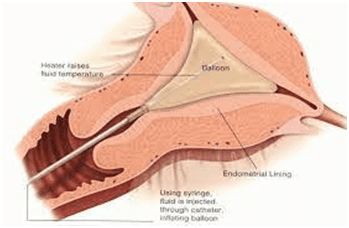
“The plasma is centrifuged again at 3300 rpm for 7 min to obtain the PRP. Then, 0.5 ml of PRP is infused into the uterine cavity with the IUI catheter (as shown above).”
“The primary outcome is endometrial expansion and the secondary outcomes are chemical and clinical pregnancies, determined by positive serum βHCG, 2 weeks after ET.

 Your Journey to Parenthood Begins with us!
Your Journey to Parenthood Begins with us!